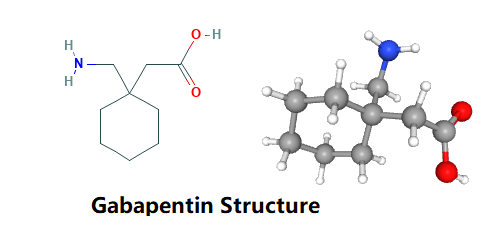
What is gabapentin?

Gabapentin is a prescription drug. It comes as an oral capsule, an immediate-release oral tablet, an extended-release oral tablet, and an oral solution.
Gabapentin oral capsule is available as the brand-name drug Neurontin. It’s also available as a generic drug. Generic drugs usually cost less than the brand-name version. In some cases, the brand-name drug and the generic version may be available in different forms and strengths.
Why it’s used
Currently, gabapentin has FDA approval for:
-
-
Postherpetic neuralgia
-
Adjunctive therapy in the treatment of partial seizures with or without secondary generalization in patients over the age of 12 years old with epilepsy, and the pediatric population, 3 to 12 year-olds with a partial seizure
-
Moderate to severe restless leg syndrome (RLS) moderate to severe
It also has off-label use for neuropathic pain, fibromyalgia, bipolar disorder, postmenopausal hot flashes, essential tremors, anxiety, resistant depressant and mood disorders, irritable bowel syndrome (IBS), alcohol withdrawal, postoperative analgesia, nausea and vomiting, migraine prophylaxis, headache, interstitial cystitis, painful diabetic neuropathy, social phobia, generalized tonic-clonic seizures, pruritus (itching), insomnia, post-traumatic stress disorder (PTSD), and refractory chronic cough.
Gabapentin oral capsule is used to treat the following conditions:
-
- Seizures: Gabapentin is used to treat partial (focal) seizures. It’s taken together with other seizure medications in adults and in children 3 years of age and older who have epilepsy.
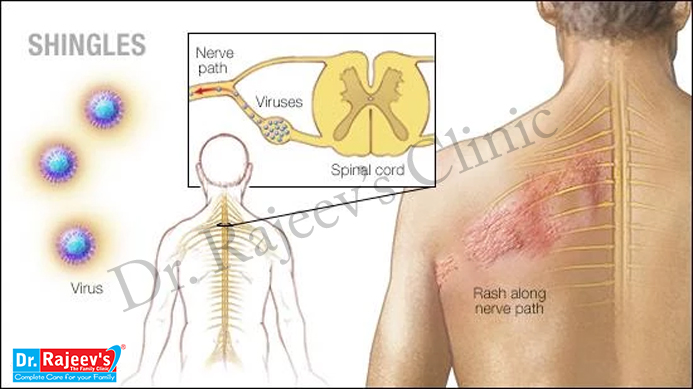
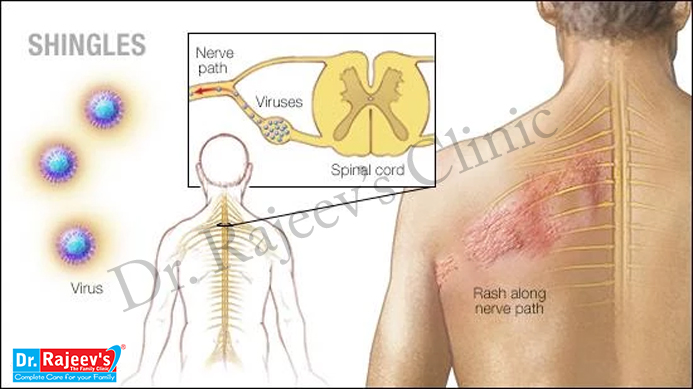
- Postherpetic neuralgia: This is pain from nerve damage caused by shingles, a painful rash that affects adults. Shingles appears after infection with the varicella zoster virus. This virus occurs in people who have had chicken pox.
Nerve pain can be a symptom of many different conditions, including cancer, HIV, diabetes, and shingles. For some, nerve pain is frustrating; for others, nerve pain is devastating and life-changing.

Whether it feels like burning, pinpricks, or sudden shocks of electricity, nerve pain can disrupt your life at home and at work. It can limit your ability to get around. Over time, it can grind you down. Studies show that people with nerve pain have higher rates of sleep problems,anxiety, and depression.Your nervous system is involved in everything your body does, from regulating your breathing to controlling your muscles and sensing heat and cold.
There are three types of nerves in the body:
-
- Autonomic nerves. These nerves control the involuntary or partially voluntary activities of your body, including heart rate, blood pressure, digestion, and temperature regulation.
- Motor nerves. These nerves control your movements and actions by passing information from your brain and spinal cord to your muscles.
- Sensory nerves. These nerves relay information from your skin and muscles back to your spinal cord and brain. The information is then processed to let you feel pain and other sensations.
Because nerves are essential to all you do, nerve pain and damage can seriously affect your quality of life.
When you have a serious medical condition such as cancer or HIV, dealing with the additional misery of nerve pain can be especially hard. But there is good news. While nerve pain can’t always be cured, it can be treated — and there are a lot of good options available.
Experts believe that 40 million Americans are living with nerve pain. The impact of nerve pain is tremendous. Both the costs to the healthcare system as well as loss of wages and productivity are staggering.
What is Postherpetic Neuralgia ?
Postherpetic neuralgia (post-hur-PET-ik noo-RAL-juh) is the most common complication of shingles. The condition affects nerve fibers and skin, causing burning pain that lasts long after the rash and blisters of shingles disappear.
The chickenpox (herpes zoster) virus causes shingles. The risk of postherpetic neuralgia increases with age, primarily affecting people older than 60. There’s no cure, but treatments can ease symptoms. For most people, postherpetic neuralgia improves over time.
How Are Nerve Pain and Nerve Damage Treated?
In many instances, nerve damage cannot be cured entirely. But there are various treatments that can reduce your symptoms. Because nerve damage is often progressive, it is important to consult with a doctor when you first notice symptoms. That way you can reduce the likelihood of permanent damage.
Often, the first goal of treatment is to address the underlying condition that’s causing your nerve pain or nerve damage. This may mean:
-
- Regulating blood sugar levels for people with diabetes
- Correcting nutritional deficiencies
- Changing medications when drugs are causing nerve damage
- Physical therapy or surgery to address compression or trauma to nerves
- Medications to treat autoimmune conditions
Additionally, your doctor may prescribe medications aimed at minimizing the nerve pain you are feeling. These may include:
-
- Pain relievers
- Tricyclic antidepressants
- Certain anti-seizure drugs – Gabapentin
Complementary and alternative approaches may also help alleviate your nerve pain and discomfort. These include:
-
- Acupuncture
- Biofeedback
- Hypnosis
- Meditation
Dosage for postherpetic neuralgia
Adult dosage (ages 18–64 years)
-
- Typical starting dosage: Day 1, 300 mg; day 2, 600 mg (300 mg two times per day, spaced evenly throughout the day); day 3, 900 mg (300 mg, three times per day, spaced evenly throughout the day). Your doctor may further increase your dosage after day 3.
- Maximum dosage: 1,800 mg per day (600 mg, three times per day, spaced evenly throughout the day)
Child dosage (ages 0–17 years)
Dosage for people younger than 18 years has not been established.
Senior dosage (ages 65 years and older)
Your kidney function may decrease with age. Your body may get rid of this drug more slowly. Your doctor may start you on a lower dose so that too much of this drug does not build up in your body. Too much of the drug in your body can be dangerous. Your doctor may change your dose based on how well your kidneys are working.
Gabapentin in Non-Epilepsy Neuropathic Pain like Postherpetic Neuralgia
The FDA approved gabapentin for the management of postherpetic neuralgia in adults. Recently, gabapentin underwent systemic evaluation in the management of diabetic neuropathy. In 1998, Rowbotham and his research team concluded that in 229 postherpetic neuralgia patients, gabapentin had more significant pain reduction as early as two weeks after initiating the treatment.
Furthermore, other measurements of mood, depression, anger-hostility, fatigue, and physical functioning, were more effectively managed with gabapentin compared to placebo.
During the same time, Backonja reviewed the effect of gabapentin in 165 diabetic neuropathy patients and showed the result that pain reduction in the gabapentin group is greater (as measured with an 11-point Likert scale) in comparison to the placebo group. And the results were significant from 2 weeks of initiation of therapy and stayed significant during the eight weeks of study.
Patients in the treatment group also reported improvement in their quality of life. This medication was well tolerated in 67% of patients who received a maximum daily dosage of 3600 mg.
Postherpetic neuralgia is a nerve disease occurs after an attack of herpes zoster infection. Herpes zoster or ‘shingles’ is a viral infection which affects the skin, especially sides of the chest, caused by varicella zoster virus. This is the same virus which causes chicken pox in children.
After an episode of herpes, the virus remains dormant in the nerve tissues of the body. This virus may become active when the immunity of the individual reduces or during convalescence after a major illness, resulting in blisters on the skin, known as shingles. It is accompanied with a rash which disappears without major consequences in about two to four weeks. Around 50% of individuals with shingles go on to develop post herpetic neuralgia (PHN) or after-shingles pain.
The neuralgia begins when the herpetic eruptions begin to heal. The pain appears usually in the affected dermatone or the affected nerve course and results in severe pain in the region which has the same nerve supply. The pain is a drawing, pricking type of intense pain, sometimes accompanied with burning sensation of the skin. The pain lasts from a few weeks to few months, rarely years.
Causes
-
-
- Severe rash within three days of shingles infection
- A study shows that, 65% of patients were women
- The chances of developing PHN, increases when the shingles occurs in persons over 50 years.
- The incidence of herpes zoster is up to 15 times higher in HIV-infected patients than in uninfected persons, and as many as 25 percent of patients with Hodgkin’s lymphoma develop herpes zoster.
- Blacks are one fourth as likely as whites to develop this condition.
- Site of HZ involvement
- Lower risk – Jaw, neck, sacral, and lumbar
- Moderate risk – Thoracic
- Highest risk – Trigeminal (especially ophthalmic division), brachial plexus.
Signs and symptoms:
-
- A pain that continues for 3 months or more, after the healing of shingles, is defined as PHN.
- PHN pain may be burning, aching, itching and sharp and the pain can be constant or it can come and go
- The skin which was affected with blisters, may show scarring
- The involved dermatome may show altered sensations, either hypersensitivity or reduced sensitivity.
- In rare cases, where if the nerves involved also control muscle movement, the patient might also experience muscle weakness, tremor or paralysis
Postherpetic Neuralgia Treatment:
The conventional treatment is directed at pain control while waiting for the condition to resolve. Pain therapy may include multiple interventions, such as topical medications, over-the-counter analgesics, tricyclic antidepressants, anticonvulsants and a number of non medical modalities. Occasionally, narcotics may be required.
When it comes to treating postherpetic neuralgia, you may need to take a combination of medications to effectively manage your pain and other PHN symptoms. No single treatment plan is right for everyone—what medications you take will depend on your PHN symptoms.
While symptoms differ from person to person, for most people, PHN does improve over time. Researchers found that more than half of all patients with PHN stop experiencing pain within one year.1
Fortunately, during that period of intense pain and other symptoms, there are certain medications that you can take to significantly help control postherpetic neuralgia symptoms.
Before trying a prescription medication, your doctor will most likely want you to try an over-the counter (OTC) analgesic (painkiller) medication, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs). These medications can help relieve pain and other PHN symptoms.
Tylenol is an example of acetaminophen, and Advil is an example of an NSAID you can take to help treat PHN.
Another OTC medication you may want to try for PHN is capsaicin cream. This cream—made from hot chili pepper seeds—is applied to the affected skin, and it can be helpful for reducing PHN-related pain. But this cream can be painful, so talk to your doctor about how much you should apply.
If these medications aren’t strong enough to treat your PHN symptoms, your doctor may suggest some of the prescription medications below to treat your postherpetic neuralgia.
-
- Tricyclic antidepressants, such as amitriptyline (Elavil), nortriptyline (Pamelor), and desipramine (Norpramin) are effective at treating postherpetic neuralgia pain. Other classes of antidepressant are also helpful. All classes of antidepressant take a few weeks to start working.
- Anticonvulsants, developed to control seizures, can help reduce the pain of PHN. These include gabapentin (Neurontin), carbamazepine (Tegretol) and pregabalin (Lyrica). Gabapentin enacarbil (Horizant) and gabapentin (Gralise) are approved by the FDA for the treatment of PHN in adults.
- Anti-viral drugs valacyclovir and acyclovir are also becoming medications of choice for treating postherpetic neuralgia.
- Lidocaine Patches for Postherpetic Neuralgia. Lidocaine patches are FDA-approved to treat PHN. The medication in the patch—lidocaine—can penetrate your skin and go to the nerves that are sending the pain signals. A benefit of lidocaine patches is that they don’t numb the skin.
- Prescription capsaicin patches. These patches contain a very high concentration of the chili pepper extract capsaicin. The capsaicin patch Qutenza is applied in a doctor’s office for one hour every three months.
If you have severe pain and other medications don’t work for you, your doctor may want you to try an opioid. Tramadol (eg, Ultram) is an example of a relatively weak opioid that can be used to help you manage PHN. Your doctor may have you try a weaker opioid first. Opioids, such as morphine (MS Contin), oxycodone (OxyContin), and hydrocodone (Vidocin), are also used to treat moderate to severe pain of postherpetic neuralgia.
Homoeopathic Medicine:
Mezereum – For Postherpetic Neuralgia with Intense Burning
Mezereum is rated among the best medicines for postherpetic neuralgia. It is the best-suited prescription when postherpetic neuralgic pains are violent and attended with marked burning. Mezereum is the most helpful among medicines for postherpetic neuralgia in postherpetic pains located in the face. The pain in the face may get worse while eating.
Warmth brings relief. Mezereum is also helpful during active herpes zoster where eruptions are present. The key symptoms to look out for before prescribing Mezereum during herpes zoster infection are violently itching vesicles with shining red areola and intense burning.
2. Ranunculus Bulbosus – For Pains coming in Paroxysms
Another of the prominently indicated medicines for postherpetic neuralgia is Ranunculus Bulbosus. It is indicated for sharp, shooting, postherpetic neuralgic pains that come in paroxysms.
It is also one of the top listed medicines for intercostal neuralgia following herpetic infection. Ranunculus Bulbosus is also indicated for herpes zoster when the vesicles eruptions are bluish in colour. The eruptions are attended with itching and burning symptoms which worsen on contact.
3. Rhus Tox – One of the best Medicines for Postherpetic Neuralgia
Rhus Tox also figures on the list of highly effective medicines for postherpetic neuralgia. It is one of the best medicines for postherpetic neuralgia where the pains are attended with marked restlessness. The skin is sensitive to cold air in such cases. In herpes zoster, Rhus Tox is the most preferred among medicines when the vesicles are yellowish with itching and stinging.