Gabapentin is an anticonvulsive medication which first discovered in the 1970s in Japan. Its original use was as a muscle relaxer and anti-spasmodic medication, but later, it was discovered the potential of the medication as anticonvulsive medication and as an adjunct to stronger anticonvulsants. Gabapentin is an anticonvulsant medication that got FDA approval for partial seizure therapy in 1993. Currently, gabapentin has FDA approval for:
-
-
Postherpetic neuralgia
-
Adjunctive therapy in the treatment of partial seizures with or without secondary generalization in patients over the age of 12 years old with epilepsy, and the pediatric population, 3 to 12 year-olds with a partial seizure
-
Moderate to severe restless leg syndrome (RLS) moderate to severe
-
It also has off-label use for neuropathic pain, fibromyalgia, bipolar disorder, postmenopausal hot flashes, essential tremors, anxiety, resistant depressant and mood disorders, irritable bowel syndrome (IBS), alcohol withdrawal, postoperative analgesia, nausea and vomiting, migraine prophylaxis, headache, interstitial cystitis, painful diabetic neuropathy, social phobia, generalized tonic-clonic seizures, pruritus (itching), insomnia, post-traumatic stress disorder (PTSD), and refractory chronic cough.
In one placebo-controlled, retrospective study that investigated the effects of gabapentin on about 700 patients with refractory partial seizure disorder, there was an improvement in overall well-being in patients. The effect prompted a controlled investigation of the drug in primary psychiatric conditions.
An important benefit of gabapentin is that there is no interaction with valproate, lithium, and carbamazepine. Also, gabapentin has minor side effects.
-
- A new study reports the nerve pain reliever gabapentin may be helpful in treating people with serious alcohol withdrawal symptoms.
- Some experts say gabapentin is most effective if used in combination with a benzodiazepine medication.
- Gabapentin can have serious side effects, including drowsiness and abnormal eye movements.
Gabapentin in Alcohol Withdrawal
For the first time, the DSM-V includes the diagnostic guidelines for alcohol dependency. There are a variety of severe diseases that result from or are influenced by alcohol dependence include stomach ulcers, liver issues, increased risk of heart disease, and neuropathy. Researchers assess that 3.8% of worldwide deaths result from direct or indirect effects of alcohol abuse.
While gabapentin’s mechanism of action is generally understood, it appears to be a logical pharmacologic option for treating issues involving the GABA receptor system. Gabapentin is a safe, readily available, and effective drug for alcohol-use disorder treatment, specifically for the abstinence maintenance phase. A 2014 trial bolstered the evidence base for gabapentin use in the treatment of alcohol use disorder. Results for insomnia and cravings, two symptoms of alcohol use disorder abstinence maintenance, demonstrated significant improvement with gabapentin pharmacotherapy. Gabapentin has also shown a statistical benefit when used as adjunctive therapy to naltrexone (the FDA-approved alcohol use disorder medication). It is also clear that higher doses of gabapentin, 1800 mg per day, seem to have a stronger effect on alcohol-use disorder abstinence maintenance. However, the trials investigating gabapentin as monotherapy have shown mixed results.
For gabapentin, unlike disulfiram and naltrexone, there is no need for hepatic dose adjustments. Gabapentin can also be used in patients whose renal function is below 20 mg/dl (although a dosing adjustment is needed).
In 2007, Melcolm and his team compared gabapentin to lorazepam. They concluded that there were significant reductions in self-reported sleep disturbance and daytime sleepiness in patients undergoing outpatient treatment for alcohol withdrawal.
A double-blind study investigated the use of 1200 mg/ per day gabapentin in alcohol use disorder. Specifically, the researchers found gabapentin to be superior to the benzodiazepine lorazepam in treating outpatients with moderate alcohol withdrawal. This outcome was measured by a lower chance of drinking and a superior, but clinically, similar alcohol withdrawal symptom reduction.
Can a drug used primarily to treat nerve pain and partial seizures be effective in helping ease alcohol withdrawal symptoms?
The anticonvulsant drug gabapentin is used off-label to treat alcohol-related withdrawal, cravings, anxiety, and insomnia. Although it is well tolerated and has demonstrated efficacy for mild alcohol withdrawal and early abstinence, there is concern about its potential for abuse. Gabapentin should be prescribed only as a second-line alternative to standard therapies, and only after screening for opioid or other prescription drug abuse to determine if heightened monitoring is warranted. Clinicians should be aware of gabapentin’s limitations for treating alcohol use disorder and be attentive to emerging data on risks and benefits.
A Trusted Source published this week concluded that gabapentin can relieve alcohol withdrawal symptoms but is most effective for people with a history of more severe symptoms after a few days of abstinence.
Gabapentin is known under brand names such as Neurontin, Gralise, and Horizant.
It was first developed Trusted Source in Japan during the 1970s and approved for use in the United States in 1993.
The drug was originally used as a muscle relaxer and antispasmodic medication. It’s been used off-label for other conditions.
“It has been used for detoxification — alcohol withdrawal — for many years,” said Dr. Raymond F. Anton, the study’s main author and a professor of medicine at the Medical University of South Carolina in Charleston.
“For relapse prevention, other clinical trials have had mixed results. We had published several studies suggesting it would be added to other medications with some success, but it looked like only in those with alcohol withdrawal symptoms prior to treatment,” he said.
“This study proved that gabapentin could work by itself as a relapse prevention medication, but only in this with the higher alcohol withdrawal symptoms, as predicted,” Anton told Healthline.
What the study revealed
Anton’s team looked at 90 people meeting the criteria of serious alcohol use.
Over 16 weeks, 12 of the 44 participants given gabapentin had no heavy drinking days (27 percent) compared with four (9 percent) of those participants given a placebo.
The study found mild to moderate side effects, including dizziness and some fatigue.
“Very few people had significant enough side effects to stop treatment,” Anton said. “It also improved sleep.”
Dr. Meredith Sagan, an addiction psychiatrist at Alo House Recovery Centers in Southern California, says gabapentin is most effective with benzodiazepine medications commonly used for withdrawal.
“Gabapentin cannot necessarily be used safely on its own to support such a detox,” Sagan told Healthline. “It’s always important to consult a medical professional when considering detoxifying from alcohol, as it can be very dangerous due to possible seizure and others risks.”
Individualized treatments
Sagan says the combination of medications and the timeline to take them is specific to each individual.
“Some people may need more or less medication, as well as different types and combinations, depending on their degree of alcohol consumption, in addition to other factors,” she said.
“So, although gabapentin can be a useful adjunct to the benzodiazepine category of medication for alcohol detox, it is not time to say goodbye to ‘benzos’ just yet,” Sagan said.
Benzodiazepines are also used to treat anxiety and seizures as well as to relax muscles. These medications come in many manufactured forms, including Xanax, Klonopin, Librium, Valium, and Ativan.
Participants in the South Carolina study weren’t allowed to take benzodiazepines or opioids.
“For people using gabapentin just for anxiety and not for alcohol withdrawal, gabapentin can be a good non-benzodiazepine alternative,” Sagan said.
“Gabapentin at higher doses can cause an uncomfortable withdrawal when one quits taking it. However, for some people with an addiction history, gabapentin is a safe alternative to benzodiazepines, which over the long term can be physically and psychologically addictive,” she said.
Gabapentin side effects
Common side effects of gabapentin include abnormal eye movements, clumsiness or unsteadiness, constipation, diarrhea, difficulty speaking, drowsiness, dry mouth, nausea, and vomiting.
More serious side effects — which may be more common in people with psychiatric disorders — include anger and violent behavior, increased anxiousness, depression, anxiety or irritability, mania, panic attacks, suicidal thoughts or behavior, and insomnia.
“I was prescribed gabapentin when I was struggling with my severely herniated disc,” Janine McKavish Thalblum, a resident of Dublin, California, told Healthline.
“The side effects were longer than an encyclopedia. With all the pain I was in I was borderline suicidal, so I opted not to take them, as that was one of the side effects. When the pharmacist was reading (them) before handing it over, I literally started to cry,” she explained.
Thalblum did take gabapentin for 2 days before opting out. She says she couldn’t tell if the medication contributed to her “overwhelming sense of wanting to give up.”
Andrea Johnson, a resident of Oakland, California, and her late wife, Julie, both took gabapentin for pain. They had vastly different experiences.
“She had chronic pain from her legs having been shattered in a car crash. Her doctors prescribed gabapentin about 10 years ago under its brand name of Neurontin,” Johnson told Healthline.
“She stopped it after a week because it put her into a constant dream state. She was sort of awake and could do things but without being conscious of what she was doing. When I caught her rolling a cigarette without realizing that she was doing it, I put a stop to the gabapentin and told her doctor why,” Johnson said.
Johnson’s doctor prescribed her gabapentin last year for arthritis in her hips.
“I was concerned about it because of Julie’s experience, but I didn’t get the psych effects that she did,” Johnson said. “By the end of a month, it still wasn’t having an effect on my pain either, so I stopped it.”
Gabapentin and opioids
In recent years, gabapentin has been involved in opioid overdose deaths and been dubbed “an emerging threat” in a national bulletin to law enforcement.
It’s listed as a controlled substance in some states, although officials say it’s usually not the main cause of death and not as dangerous as opioids.
Pfizer, which developed gabapentin, paid $430 million in 2004 under an agreement with government prosecutors over fraudulent claims the company was accused of making about the drug’s uses.
Anton says researchers are still looking at whether gabapentin can be used as an anti-craving drug like naltrexone.
“Right now, it is estimated that only 20 percent of individuals who might benefit from reducing or stopping drinking actually receive treatment,” Anton said.
“And, of those 20 percent, only 20 percent receive any medication-assisted treatment. The standard of care in the U.S. has historically been an AA (Alcohol Anonymous) or 12-step counseling model. While that model has helped many people, many others do not want to partake in it, or haven’t found it useful.
“Medications that can be prescribed by specialized and/or primary care providers can encourage many more people to consider treatment for their alcohol use disorder,” he added.
Gabapentin is a prescription anticonvulsant used to treat epileptic seizures, postherpetic neuralgia, and restless legs syndrome. Postherpetic neuralgia is pain caused by shingles, which can last many months after having the illness.
While the exact mechanism of action of gabapentin is not fully understood, it may work by decreasing excitatory brain signaling. This can prevent seizures and change the way the brain responds to pain signals. This medication can be found as a capsule, tablet, or oral solution.

The following 11 questions are designed to help you better understand your relationship to alcohol. They will help you to tell if it resembles abuse or addiction, or is if it closer to average.
1. Do you tend to drink more than you expected to? And for longer periods of time?
2. Do you wish you could drink less, and struggle to cut down your alcohol intake?
3. Does drinking consume much of your time? In other words, do you spend a lot of your time trying to obtain, use, or recover from alcohol hangovers?
4. Do you have very strong cravings or urges to drink? Does it feel like you “need” it to get by?
5. Does drinking cause problems for you at work, in school, or in your family obligations? Does this happen frequently?
6. If drinking does cause these social and interpersonal problems for you, do you continue to drink anyway?
7. Have you given up activities that used to be meaningful for you? For example, have you quit a sport or left friendships because you don’t seem to have the time or energy anymore?
8. Do you use alcohol even when it makes your activity physically dangerous? This could be drinking while driving, using certain prescription drugs, or working with heavy machinery.
9. Do you continue to drink even after discovering that it exacerbates, worsens, or even causes other physical or mental illnesses?
10. Are you developing a tolerance for alcohol? This could show up as a decreased effect after drinking the same quantity of alcohol that you used to use, or having to drink more and more alcohol to achieve the desired level of intoxication.
11. Have you experienced withdrawal symptoms after not drinking any alcohol for a while? These include a racing heart, trouble sleeping, shakiness, sweating, fever, restlessness, nausea, or even auditory or visual hallucinations? Does more alcohol relieve these feelings?
As an Addiction Treatment Medication
The medical research community has made great strides in synthesizing thousands of drugs over the years to treat physical ailments, mental illness, and other health conditions.
Addiction is just one of the many conditions that can be treated with specific medications. And while there are presently only a handful of FDA-approved medications used to manage substance dependence, gabapentin has been considered for off-label use for as an addiction treatment drug.
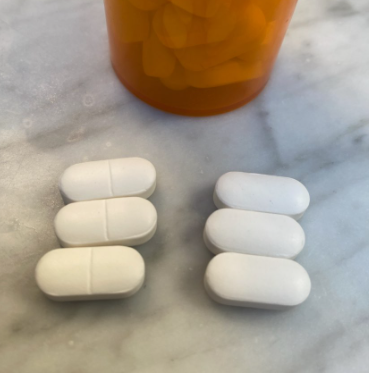
Different companies, including Parke-Davis, Greenstone, and Teva, manufacture several varieties of the generic drug. Other drugs that have been used to treat the symptoms of addiction withdrawal, for specific substances, include:
-
- Clondine
- Other anticonvulsants, such as Tegretol and Depakote
- Methadone and buprenorphine
- Naltrexone
Typical Application
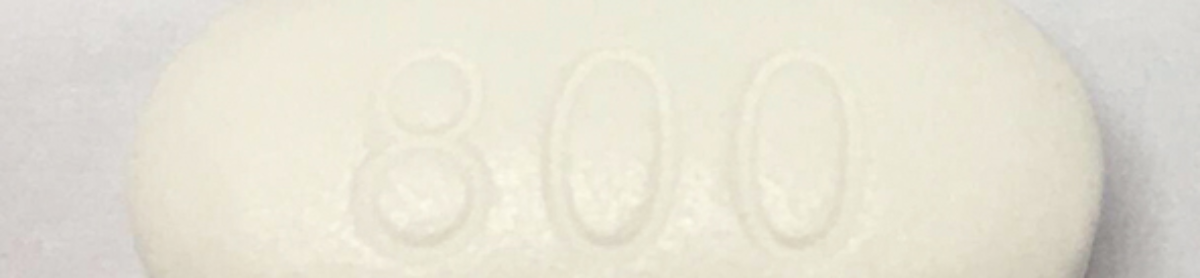
Doses range from 100 mg to 800 mg. The frequency of administration may be based on various factors such as withdrawal symptom severity and withdrawal progress. The drug’s half-life is around 5-7 hours.
Gabapentin has been evaluated for use during medical detox and throughout subsequent treatment modalities to support relapse prevention while clients adjust to their new sober lifestyles.
Treating Substance Abuse
According to Medscape, gabapentin can inflict users with suicidal thoughts and abrupt changes in behavior. For this reason, it should only be used under medical supervision. It can also cause elevated blood pressure, fever, sleep problems, appetite changes, and chest pain.
While it has been used to treat addictions to other substances, gabapentin is most often used to treat alcoholism — an addiction some 16.6 million adults suffered from in 2013, per the National Institute on Alcohol Abuse and Alcoholism.
During withdrawal from alcohol abuse or dependency, clients may experience anxiety, tremors, agitation, and irritability. In order to understand how gabapentin works, there must be a basic understanding of how the brain works first. A balance of excitatory and inhibitory nervous system activity is, in part, mediated by neurotransmitters known as GABA and glutamate. Gabapentin may work by potentiating the inhibitory signaling of GABA and reducing the neural excitation associated with glutamate activity. As a result, signals for pain, agitation, and anxiety are reduced, too.
An American Journal of Psychiatry study showed impressive results during the 16-week treatment of 150 people who were dependent on alcohol, noting better results among those who were treated with both gabapentin and naltrexone than the latter alone. The Journal of Clinical Psychiatry reported on another study in which individuals treated for alcoholism with gabapentin showed a significant reduction in how much they drank and a greater rate of abstinence than those in the placebo group.
Gabapentin may have a similar calming effect on individuals who are detoxing from marijuana and benzodiazepines. Despite claims from fans of the plant-based drug, marijuana is indeed addictive. In 2012, 305,560 people checked into rehab citing cannabis as their primary drug of abuse, per the Substance Abuse and Mental Health Services Administration. One Neuropsychopharmacology study that analyzed the use of gabapentin in the treatment of marijuana addiction and withdrawal noted individuals in the gabapentin treatment group used less marijuana, had fewer withdrawal symptoms, and experienced improvements in cognitive functioning, compared to the placebo group.
While not quite as prevalent as a substance of abuse, benzodiazepines still accounted for 17,019 admissions to treatment in 2012, per SAMHSA. Individuals who have been abusing marijuana or benzodiazepines for a long period of time may have difficulty achieving a state of relaxation without those drugs, and gabapentin can help individuals remain calm while they’re recovering from addiction.